Primary PPO Network
Logro Network’s high-performance network saves on healthcare costs while improving outcomes for employers and employees.
What is the LogroNetwork Primary PPO?
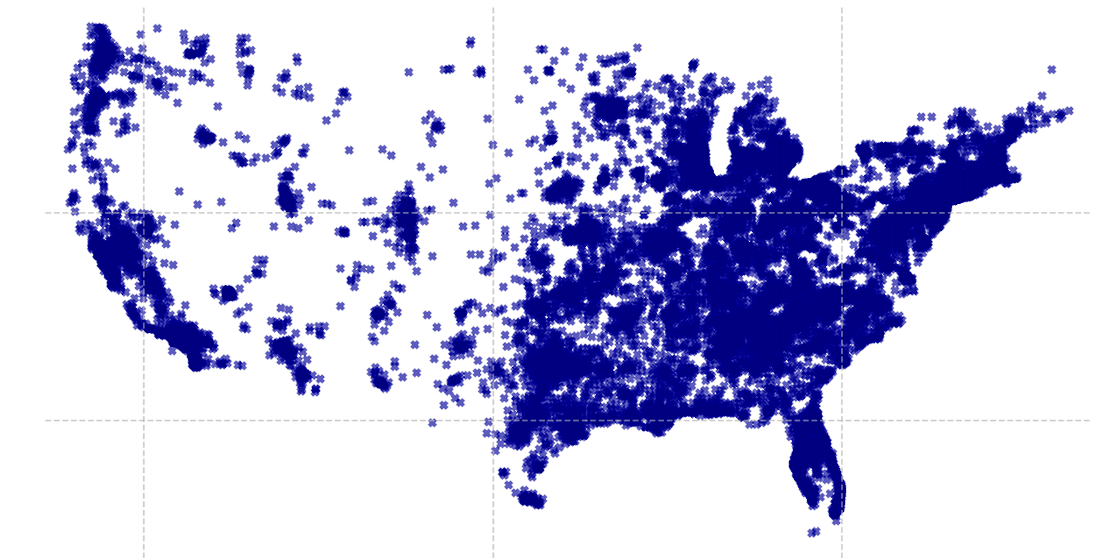
LogroNetwork is America’s first nationally credentialed, high-performance PPO built on provider-level quality and outcome metrics. As the preferred choice for self-insured employer health plans, third-party administrators, and payors, LogroNetwork combines broad access, clinical excellence, and measurable savings—without compromising flexibility or administrative simplicity.
Benefits of the LogroNetwork Primary PPO
Unmatched Provider Access and Proven Savings
The LogroNetwork PPO includes over 1.2 million credentialed providers across the country:
1M+ physicians and practitioners
4,600+ acute care hospitals
92,000+ ancillary facilities and service centers
Thanks to our outcomes-based provider selection and pre-negotiated rates, average savings per claim type include:
Practitioners: 40–45%
Inpatient: 25–30%
Outpatient: 20–25%
Ancillary: 40–50%
Credentialed Quality, Verified Outcomes
Our credentialing process, aligned with nationally recognized standards, ensures only high-performing, cost-efficient providers are admitted into the LogroNetwork. Our network emphasizes treatment appropriateness, care outcomes, and total cost efficiency—not just participation. Providers are reviewed using robust analytics and recredentialed regularly to maintain excellence in care delivery.
Flexible, Customizable, and Easy to Administer
Whether used as a national PPO solution or to extend another network’s reach, LogroNetwork can be customized by:
Geography (national or regional carve-outs)
Specialty or provider type
Tiered benefit design or wrap solutions
Integration with cost containment, navigation, and steerage solutions
All with single-claim submission simplicity, streamlined implementation, and full compliance support.